-

 Alma Murphy MD PC
Alma Murphy MD PC
Eye Physician & Surgeon
490 N Alvernon Way
Tucson, AZ 85711
(520) 323-1313
eyesaz.com -

 Alma Murphy MD PC
Alma Murphy MD PC
Eye Physician & Surgeon
490 N Alvernon Way
Tucson, AZ 85711
(520) 323-1313
eyesaz.com -

 Alma Murphy MD PC
Alma Murphy MD PC
Eye Physician & Surgeon
490 N Alvernon Way
Tucson, AZ 85711
(520) 323-1313
eyesaz.com -

 Alma Murphy MD PC
Alma Murphy MD PC
Eye Physician & Surgeon
490 N Alvernon Way
Tucson, AZ 85711
(520) 323-1313
eyesaz.com
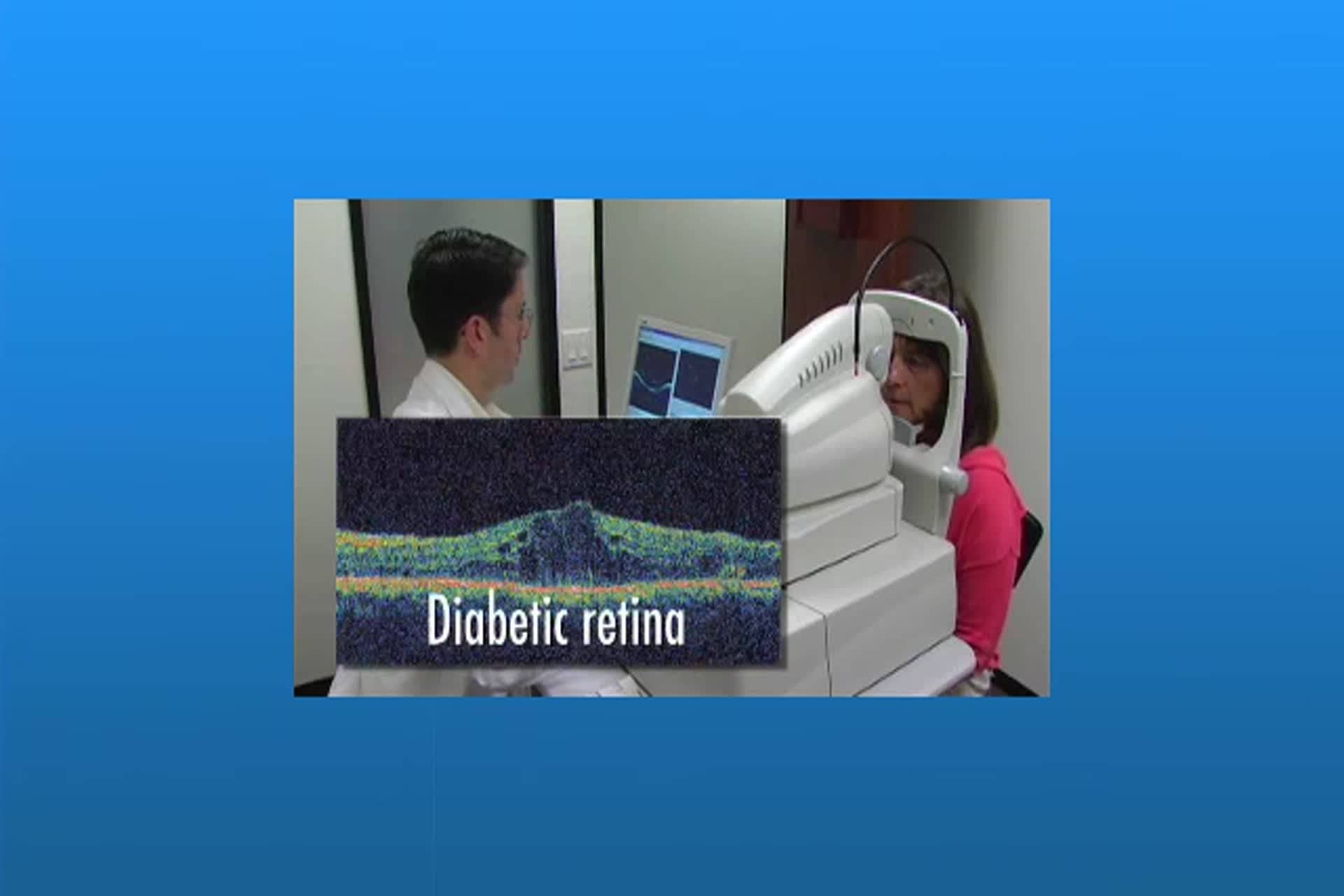
Diabetes and Diagnosis of Diabetic Retinopathy
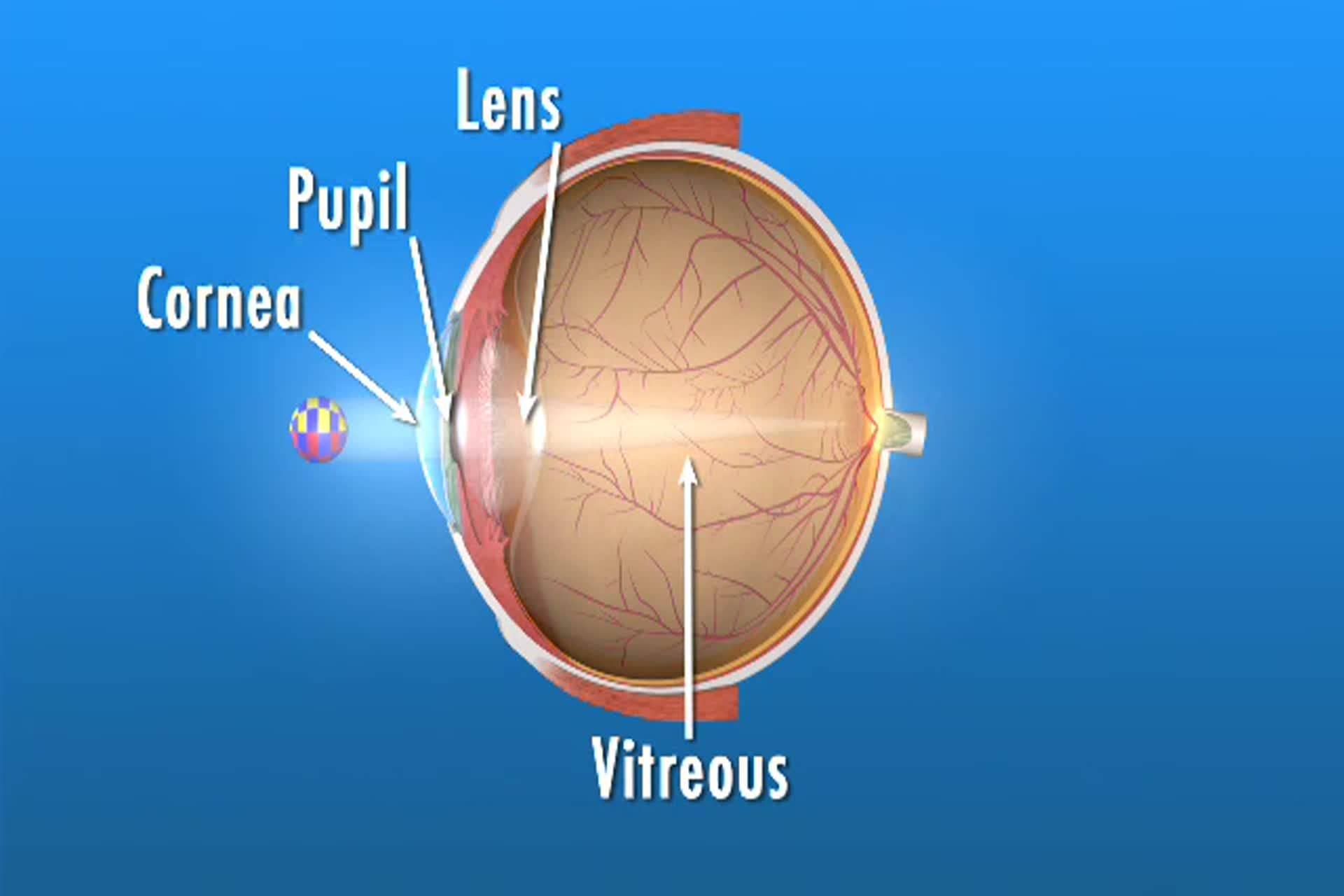
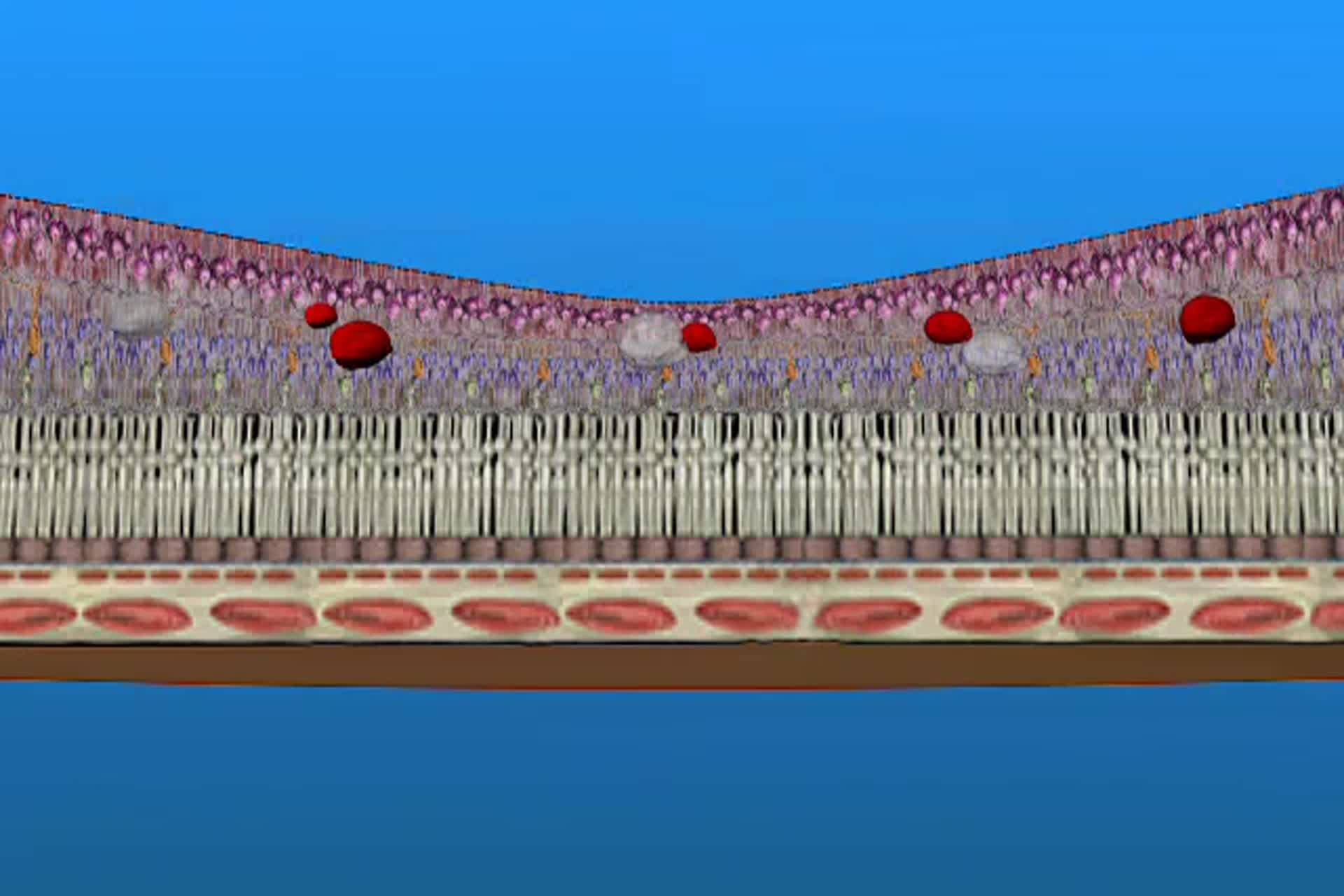
Diabetes can affect your eye health and vision by damaging the retina and also leading to the formation of cataracts.